
We developed an end-to-end claims processing digitization solution to reduce manual efforts and empower predominant health insurer with Gen AI driven automationsdata

A prominent player in India's thriving health insurance landscape, the client is a leading company offering a diverse range of specialized products. They provide a broad spectrum of health insurance benefits, for all types of hospitalizations, access to advanced medical treatments, and cover for AYUSH treatments.
The company wants to harness automation to streamline the intricate process of data extraction and classification from medical documents. This strategic initiative aims to enhance operational efficiency and deliver unparalleled customer experience.
Customer is facing critical challenges in their claim processing workflow, hindering efficiency and accuracy. Key obstacles include:
They want to implement an intelligent, automated system capable of handling diverse document formats, extracting relevant data with high accuracy, and employing advanced analytics for smarter claim processing.
Ganit has made a significant dent in various industries using data science and analysis. Ganit partners with clients to translate their data into a tangible, insightful plan of action that delivers on a measurable impact to the clients’ topline & bottom-line growth.
With a strong Gen AI practice and a dedicated Gen AI Centre of Excellence (CoE), Ganit has advanced capabilities in building consumable Gen AI driven solutions for our customers. With almost 20 demos catering to different industry verticals and business functions, Ganit has a proven track of delivering customer delight through accelerated implementation.
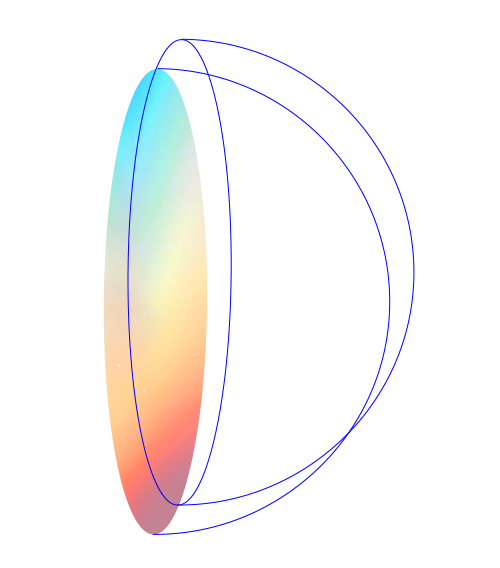
Using the power of machine learning and cloud computing, a scalable AI-powered automated claims processing system was developed, leveraging AWS services to revolutionize their workflow.
See the impact that we make on our
cross-industry client base.
 Top
Top